Pelvic congestion syndrome, or PCS, is a cause of chronic pelvic pain in women. The pain and pressure from PCS is worse with standing or sitting for a long time. It can also be painful to have intercourse.
PCS develops when blood backs up and pools in the pelvic veins, causing them to stretch out. These dilated veins can also appear in the thighs, buttocks or vaginal area. They can look like the varicose veins that some people develop in their legs.
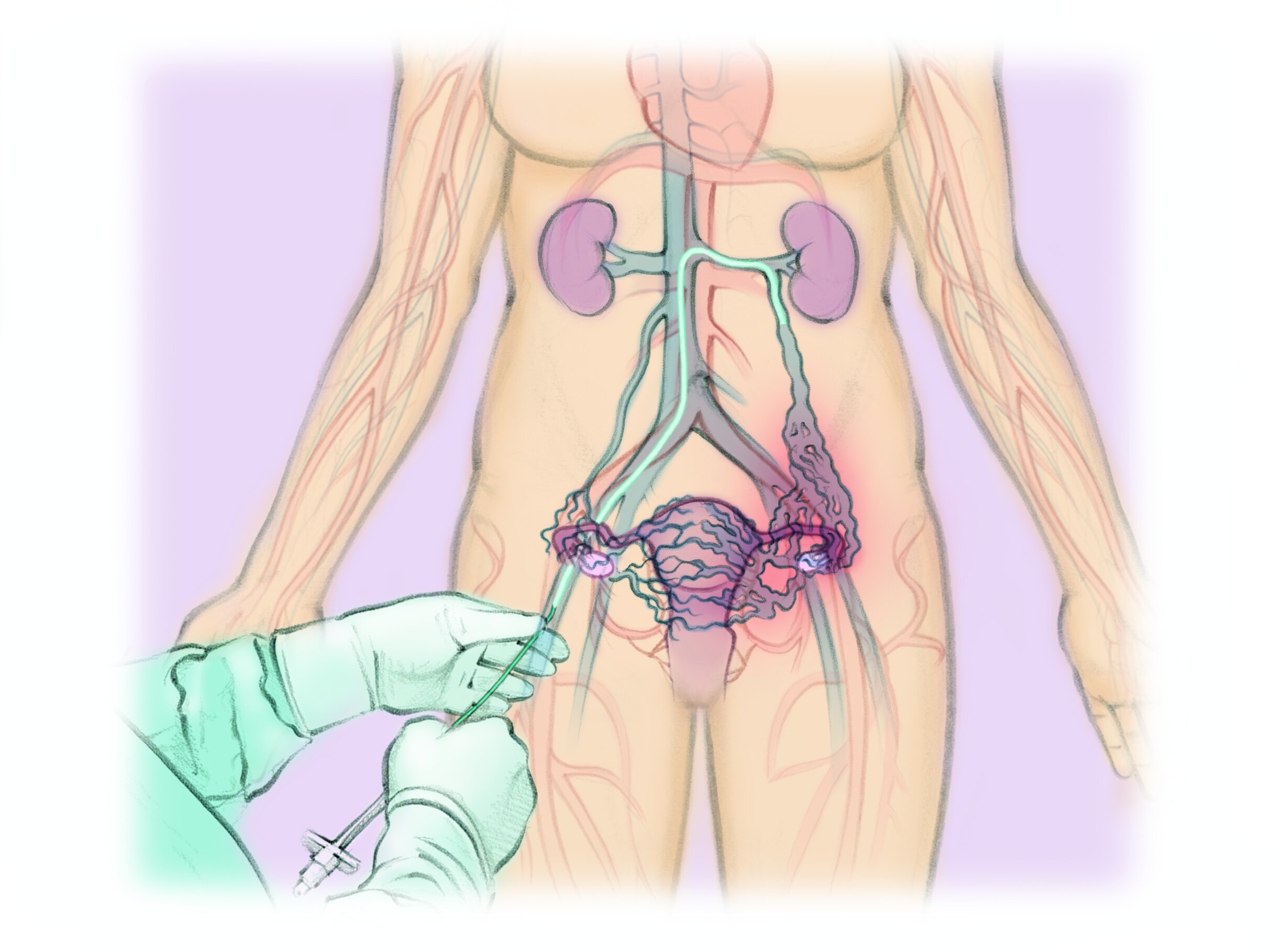
PCS can be treated by “gonadal vein embolization,” a minimally invasive procedure to block the unhealthy veins from the inside. This decreases the pressure and relieves most or all of the symptoms of PCS in 8-9 in 10 women.
What is PCS and Gonadal Vein Embolization?
How is Gonadal Vein Embolization done?
You will be given medicines to help you relax. The clinician will numb the skin on your neck or upper thigh. They will thread a thin tube through the skin into a large vein. Moving x-rays will guide the clinician as they move the small tube into the unhealthy veins in the pelvis. The clinician will inject special material into the unhealthy veins to block them and encourage the blood to flow through your healthy veins, instead. The tube will be removed and a dressing placed over where the tube entered the skin.
Gonadal Vein Embolization
1. The clinician numbs the skin of the neck or upper thigh.
2. They use moving x-rays to guide a thin tube into the abnormal veins in the pelvis. The clinician injects special materials into the abnormal veins to close them off
3. After, they remove the tube and put a bandage over the pinhole in the skin.
What are the risks?
Gonadal vein embolization is generally a safe procedure when done by a specialist.
Blocking the unhealthy veins can irritate them, which can cause temporary pain and fever.
The unhealthy veins can come back or symptoms do not improve in 1 in 10 woman.
The special material used to block the vein can go somewhere else in the body in 1-2 in 100 women. This can cause symptoms or no symptoms depending on where the material ends up.
Other rare complications include bleeding or infection at the wound site.
The procedure DOES NOT affect the menstrual cycle or fertility. It does use radiation. Even though the radiation dose is very small, it could harm the ovaries.
What are the alternatives?
Your treatment options depend on your preferences and your unique conditions.
Alternative 1 No treatment. The abnormal veins and chronic pelvic pain are not likely to get better on their own.
Alternative 2 Surgery. A surgeon can tie off the dilated veins or remove them during surgery. This has slightly less risk of the veins coming back and slightly more risk of other complications. It requires longer recovery.
Frequently asked questions
Why do I have chronic pelvic pain?
Pain in the lower abdomen or pelvis lasting more than 6 months can have several different causes. In some women, it may be the result of high blood pressure in the veins of pelvis. This is called pelvic congestion syndrome (PCS).
What are the symptoms of pelvic congestion syndrome?
Pelvic pain or pressure lasting more than 6 months
Pelvic pain that is worse with standing or sitting for a long time
Dilated, visible varicose veins in the thighs, buttocks or vaginal area
What causes pelvic congestion syndrome?
Veins normally carry blood from the body back to the heart. Veins normally have valves that help keep the blood flowing in its usual direction back to the heart. Without working valves, the blood can flow backwards and pool in the veins, causing them to stretch and bulge.
How is pelvic congestion syndrome diagnosed?
Your doctor may examine you, do a Pap smear to rule out cervical cancer, and order routine blood tests. Your doctor may order an imaging test like an ultrasound, MRI or a CT scan. Pelvic congestion syndrome can be difficult to diagnosis.
How is pelvic congestion syndrome treated?
Pelvic congestion syndrome can be treated with a same-day minimally invasive, image-guided procedure (MIIP) to block the unhealthy veins from the inside and prevent blood from pooling in the veins of the pelvis. This procedure is performed by an Interventional Radiologist (IR), who specializes in these procedures.
How can I prepare for my MIIP?
Before your procedure, you may be asked:
to stop taking medicines that could make you bleed (examples: aspirin, blood thinners, vitamin E, ibuprofen)
to not eat or drink after midnight the day of your treatment
to talk with your doctor if you take insulin for diabetes
What is the MIIP to treat pelvic congestion syndrome like?
A nurse will start an IV in your arm.
You will change into a gown for the procedure.
You will lie on a table in a special procedure room equipped to take live x-ray pictures.
You will get medicine in your IV to make you comfortable and drowsy. You will still be able to speak and breathe on your own.
Your skin will be cleaned and prepared.
After numbing the skin, the IR will put a thin plastic tube the size of spaghetti into the vein of your upper thigh.
The IR will guide the plastic tube into the dilated veins inside of your pelvis while watching with x-rays.
The IR doctor will take x-ray pictures of the veins after injecting contrast dye into them.
The IR will use a special material to block the problem veins so they cannot cause pain.
The IR will remove the tube and put a bandage over the nick. No stitches are needed.
The procedure usually takes 30 minutes to 2 hours.
What should I expect after my MIIP?
You will stay in the hospital bed for several hours for observation. Your IV will be removed and you will be allowed to go home at the end of the day.
You may experience pelvic pain the first 3 days after the treatment. This pain can be treated successfully with just oral pain medicines in up to 85% of patients.
What are the risks?
The MIIP to treat pelvic congestion syndrome is considered to be very safe. Complications are rare and the risks are the same for any procedure:
Bleeding
Infection
Damage to surrounding tissues
Your IR will discuss the risks and benefits with you before your MIIP.
For more information about treating pelvic congestion syndrome: